Guided Bone Regeneration (GBR) is a pivotal surgical procedure designed to restore lost bone in the jaw. Whether you’re preparing for a dental implant or addressing a bone defect, understanding GBR is essential for achieving optimal oral health and long-term stability.
Understanding Guided Bone Regeneration
Guided Bone Regeneration is a sophisticated technique used to promote the growth of new bone in areas where it has been lost or is insufficient. This process is integral to various dental and orthopedic applications, ensuring that bone defects are effectively managed and bone volume is adequately restored.
What is Guided Bone Regeneration?
- Definition: GBR involves the use of barrier membranes to direct the growth of bone and prevent the invasion of soft tissues into the regeneration site.
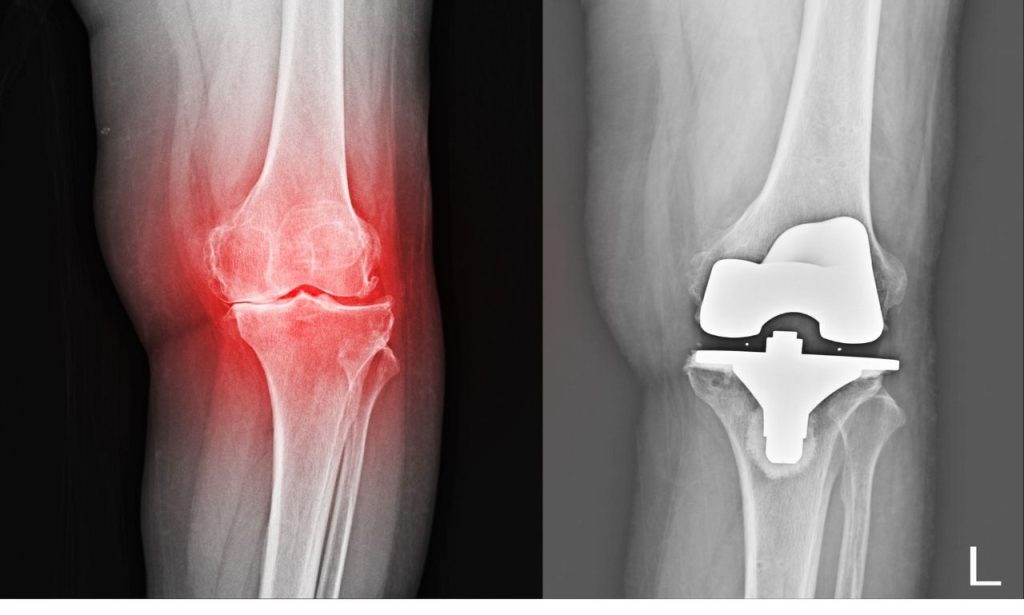
- Purpose: Primarily utilized to rebuild bone structure, GBR ensures a stable foundation for dental implants or repairs bone defects caused by trauma, periodontal disease, or tooth extraction.
Mechanism of GBR
- Barrier Function: The barrier membrane acts as a shield, allowing only bone-forming cells to populate the area, thereby facilitating targeted bone growth.
- Cellular Interaction: GBR enhances the migration of osteoprogenitor cells to the defect site, promoting effective bone regeneration and integration with existing bone structures.
Importance of Guided Bone Regeneration
GBR plays a crucial role in modern dentistry and maxillofacial surgery by addressing bone loss and ensuring the success of various dental procedures. Its significance extends beyond mere bone restoration, impacting both functional and aesthetic aspects of oral health.
Enhancing Dental Implant Success
- Stable Foundation: GBR provides the necessary bone volume and density required for the secure placement of dental implants, ensuring they remain firmly anchored.
- Long-term Stability: By restoring bone structure, GBR reduces the risk of implant failure, promoting the longevity and effectiveness of osseointegrated implants.
Managing Bone Defects
- Traumatic Injuries: GBR repairs bone loss resulting from accidents or surgical removal of tumors, restoring structural integrity and function.
- Periodontal Disease: Advanced gum disease can lead to significant bone loss; GBR counteracts this by regenerating bone and preserving the oral structure.
Aesthetic and Functional Restoration
- Facial Structure: Maintaining bone volume helps preserve facial symmetry and prevents sunken appearances caused by bone resorption.
- Chewing Efficiency: Restored bone volume ensures better chewing efficiency and overall oral functionality, enhancing the quality of life.
Types of Membranes Used in GBR
Membranes are the cornerstone of GBR, serving as barriers that guide bone regeneration. They are broadly categorized into resorbable and non-resorbable membranes, each with distinct properties and applications.
Resorbable Membranes
Resorbable membranes are designed to degrade naturally within the body, eliminating the need for a second surgery to remove them.
- Biodegradable Materials: Commonly made from collagen or synthetic polymers like polylactic acid (PLA) and polyglycolic acid (PGA).
- Advantages:
- No need for additional surgical procedures for membrane removal.
- Lower risk of membrane exposure and subsequent infection.
- Common Types:
- Collagen Membranes: Naturally derived, biocompatible, and promote tissue regeneration.
- Synthetic Polymers: Engineered for controlled degradation rates, providing sustained support during bone healing.
Non-Resorbable Membranes
Non-resorbable membranes provide long-term support for bone regeneration but require a second surgery for removal if necessary.
- Permanent Barriers: Typically made from materials like titanium mesh or expanded polytetrafluoroethylene (ePTFE).
- Advantages:
- Offer prolonged support, ideal for larger or more complex bone defects.
- Provide a stable framework for bone growth over extended periods.
- Challenges:
- Require additional surgical intervention for removal.
- Higher risk of complications such as membrane exposure, which can lead to infections.
Procedural Steps in Guided Bone Regeneration
Executing GBR involves a series of meticulous steps to ensure successful bone regeneration. Each phase is critical in promoting optimal outcomes and minimizing complications.
Initial Assessment

- Comprehensive Evaluation: Conducting clinical examinations, radiographic imaging, and assessing bone quality and quantity to determine the extent of bone loss.
- Planning: Determining the appropriate graft materials, selecting the type of membrane, and outlining the surgical protocol tailored to the patient’s specific needs.
Surgical Site Preparation
- Anesthesia: Administering local or general anesthesia to ensure patient comfort throughout the procedure.
- Incision and Flap Design: Creating precise incisions to access the bone defect while preserving surrounding soft tissues and minimizing trauma.
Membrane Placement
- Barrier Installation: Positioning the chosen membrane over the bone defect to guide and contain bone regeneration.
- Fixation: Securing the membrane with pins or sutures to prevent movement during the healing process, ensuring the barrier remains intact.
Bone Grafting Procedures
- Bone Graft Selection: Choosing the appropriate bone graft material, such as autogenous bone grafts, allografts, xenografts, or synthetic grafts, based on the defect size and patient requirements.
- Placement: Carefully placing the graft material within the defect to provide a scaffold for new bone growth and support the regeneration process.
Closure and Suturing
- Flap Repositioning: Carefully closing the surgical site to protect the membrane and graft, ensuring a secure environment for healing.
- Suturing Techniques: Utilizing tension-free suturing to promote optimal healing and minimize the risk of membrane exposure or complications.
Clinical Indications for GBR
GBR is versatile and applicable in various clinical scenarios to address bone deficiencies and support dental treatments, making it a fundamental technique in dental and maxillofacial surgery.
Dental Implant Placement
- Bone Volume Enhancement: Ensuring adequate bone mass and density for the stable placement of dental implants, crucial for their long-term success.
- Predictable Outcomes: Increasing the success rates of osseointegrated implants by providing a robust foundation through effective bone regeneration.
Bone Defects Management
- Traumatic Bone Loss: Repairing defects caused by accidents, surgical interventions, or congenital anomalies, restoring structural integrity.
- Cranial Defects: Addressing bone loss in the cranial region, ensuring the preservation of structural and functional integrity.
Periodontal Disease
- Bone Preservation: Counteracting bone resorption associated with advanced gum disease, preserving the oral structure and preventing further bone loss.
- Functional Restoration: Maintaining the integrity of the oral cavity and supporting surrounding teeth, enhancing overall oral health.
Biological Mechanisms of GBR
Understanding the biological processes behind GBR is essential for optimizing treatment outcomes and enhancing bone regeneration. These mechanisms involve intricate interactions at the cellular and molecular levels.
Role of Growth Factors
Growth factors play a crucial role in GBR by stimulating cellular activities that promote bone formation and healing.
- Osteoinduction: Proteins like bone morphogenetic proteins (BMPs) induce the differentiation of progenitor cells into osteoblasts, essential for new bone formation.
- Angiogenesis: Growth factors promote the formation of new blood vessels, ensuring a sufficient nutrient supply and waste removal, which are vital for healthy bone regeneration.
Bone Healing Processes

The bone healing process in GBR involves several phases that collectively contribute to effective bone regeneration.
- Inflammatory Phase: The initial response to surgery, involving clot formation and the recruitment of immune cells to the surgical site.
- Proliferative Phase: Formation of new bone matrix and angiogenesis, setting the foundation for new bone growth.
- Remodeling Phase: Maturation and strengthening of the newly formed bone structure, integrating it with the existing bone.
Bone Graft Materials Used in GBR
Selecting the right bone graft material is critical for successful GBR. Materials are categorized based on their origin and properties, each offering distinct advantages and considerations.
Autogenous Grafts
Autogenous grafts are harvested from the patient’s own body, offering the highest compatibility and osteogenic potential.
- Definition: Grafts sourced from the patient’s iliac crest, mandibular ramus, or other skeletal sites.
- Advantages:
- Superior osteogenic potential due to the presence of living cells and growth factors.
- No risk of immune rejection, as the graft is autologous.
- Disadvantages:
- Requires a secondary surgical site, increasing overall procedure time and potential discomfort.
- Limited availability, especially in cases requiring large grafts.
Allografts
Allografts are obtained from human donors and processed to ensure safety and compatibility.
- Definition: Grafts sourced from cadaveric donors, typically processed and sterilized to eliminate disease transmission risks.
- Advantages:
- Abundant supply, making them suitable for extensive bone defects.
- No additional surgical site required, reducing patient discomfort.
- Disadvantages:
- Risk of disease transmission, although minimized through stringent processing protocols.
- Potential for immune response, which may affect graft integration.
Xenografts
Xenografts are derived from animal sources, commonly bovine bone, and used as scaffolds for new bone growth.
- Definition: Grafts sourced from animals, typically bovine, treated to remove organic components and ensure biocompatibility.
- Advantages:
- High availability and consistency in quality.
- Excellent scaffold properties that support new bone growth.
- Disadvantages:
- Risk of immune reaction, albeit low due to extensive processing.
- Longer integration time compared to autografts, potentially prolonging the healing process.
Synthetic Grafts
Synthetic grafts are man-made materials engineered to mimic the properties of natural bone, offering customizable options for GBR.
- Definition: Materials such as hydroxyapatite, tricalcium phosphate, and bioactive glass designed to support bone regeneration.
- Advantages:
- Highly biocompatible and customizable in terms of porosity and degradation rates.
- No risk of disease transmission or immune rejection.
- Disadvantages:
- Limited osteogenic potential compared to autografts, often requiring the addition of growth factors.
- May not integrate as seamlessly with natural bone, potentially affecting long-term stability.
Aftercare and Healing Process
Proper post-operative care is essential to ensure the success of GBR and facilitate optimal bone regeneration. Adhering to aftercare protocols minimizes the risk of complications and promotes effective healing.
Post-Operative Care
- Oral Hygiene: Maintaining meticulous oral hygiene to prevent infection and promote a clean healing environment.
- Dietary Restrictions: Consuming a soft diet to minimize stress on the surgical site and avoid dislodging graft materials.
- Medications: Taking prescribed antibiotics and pain relievers as directed to manage pain and prevent infection.
Signs of Complications
Recognizing early signs of complications is crucial for timely intervention and ensuring successful bone regeneration.
- Infection: Indicators include redness, swelling, increased pain, and discharge at the surgical site.
- Membrane Exposure: Visible membrane through the gum tissue increases the risk of contamination and may necessitate additional surgical procedures.
- Delayed Healing: Persistent pain, swelling, or lack of bone growth may indicate underlying issues requiring medical attention.
Success Rates and Outcomes of GBR
Guided Bone Regeneration boasts high success rates when performed correctly, leading to significant improvements in bone volume and implant stability. Its predictable outcomes make it a preferred choice in various clinical scenarios.
Predictable Bone Regeneration
- Consistent Outcomes: Utilizing appropriate materials and techniques ensures reliable restoration of bone volume and structure.
- Long-term Stability: Enhanced bone architecture supports the longevity of dental implants and other oral restorations, reducing the risk of implant failure.
Aesthetic and Functional Benefits
- Enhanced Smile: Improved bone structure contributes to a more natural and aesthetically pleasing appearance, boosting patient confidence.
- Improved Functionality: Restored bone volume ensures better chewing efficiency and overall oral functionality, enhancing the quality of life.
Risks and Complications of GBR
While GBR is generally safe and effective, it is not without potential risks and complications. Being aware of these can help in taking preventive measures and ensuring successful outcomes.
Common Risks
- Infection: Bacterial invasion of the surgical site can compromise the graft and hinder bone regeneration.
- Membrane Exposure: Exposure of the membrane increases the risk of infection and may require additional surgical intervention.
- Graft Rejection: Although rare, the body may reject the graft material, impeding bone regeneration and necessitating alternative treatments.
Mitigating Risks
- Proper Surgical Technique: Ensuring meticulous execution of the procedure minimizes the likelihood of complications and enhances the success of GBR.
- Post-Operative Care: Adhering to aftercare instructions promotes healing and reduces the risk of infections and other complications.
- Regular Follow-Ups: Monitoring progress through scheduled appointments allows for early detection and management of any issues, ensuring optimal outcomes.
Additional Considerations in Guided Bone Regeneration
To further enhance the effectiveness of GBR, several additional factors and advanced techniques can be considered. These elements contribute to the overall success and longevity of bone regeneration procedures.
Ridge Preservation
Ridge preservation techniques are employed to maintain the alveolar ridge following tooth extraction, preventing significant bone loss and facilitating future GBR procedures.
- Procedure: Involves placing bone graft materials and barrier membranes immediately after tooth extraction to preserve bone volume.
- Benefits: Minimizes the extent of bone loss, simplifies subsequent GBR, and enhances the success rate of dental implants.
Horizontal and Vertical Ridge Augmentation
Addressing both horizontal and vertical bone deficiencies is essential for comprehensive bone regeneration and optimal implant placement.
- Horizontal Ridge Augmentation: Involves widening the alveolar ridge to accommodate implants and improve aesthetic outcomes.
- Vertical Ridge Augmentation: Focuses on increasing the height of the alveolar ridge, providing sufficient bone volume for implant stability.
Advanced Grafting Techniques
Incorporating advanced grafting techniques can enhance the predictability and effectiveness of GBR.
- Bone Morphogenetic Proteins (BMPs): Utilizing BMPs to stimulate osteoinduction and promote bone formation.
- 3D Scans and Custom Membranes: Employing 3D imaging to create customized membranes and grafts tailored to the patient’s specific anatomy, improving fit and integration.
Emerging Research and Clinical Studies
Ongoing research and clinical studies continue to refine GBR techniques and materials, enhancing outcomes and expanding clinical applications.
- Comparative Studies: Evaluating the effectiveness of different graft materials and membrane types to determine the most suitable options for various clinical scenarios.
- Experimental Models: Utilizing animal models and in vitro studies to explore new materials and techniques, advancing the field of bone regeneration.
Bone Regeneration Process in Detail
Delving deeper into the bone regeneration process elucidates the intricate steps and factors that contribute to successful GBR outcomes. Understanding these processes can aid in optimizing treatment protocols and enhancing clinical success rates.
Cellular and Molecular Events
Bone regeneration involves a cascade of cellular and molecular events that facilitate the formation of new bone tissue.
- Osteoprogenitor Cells: These precursor cells differentiate into osteoblasts, the cells responsible for bone formation.
- Extracellular Matrix Formation: Osteoblasts produce the extracellular matrix, providing a scaffold for mineral deposition and bone tissue formation.
- Mineralization: Calcium and phosphate ions precipitate to form hydroxyapatite crystals, strengthening the newly formed bone matrix.
Role of Connective Tissue
Connective tissue plays a supportive role in GBR by providing a framework for cell migration and nutrient transport.
- Fibroblast Activity: Fibroblasts produce collagen fibers that form the structural matrix for tissue regeneration.
- Vascularization: The formation of new blood vessels ensures an adequate supply of nutrients and oxygen, essential for bone healing and regeneration.
Mechanical Stability
Maintaining mechanical stability at the regeneration site is crucial for effective bone healing and integration.
- Membrane Fixation: Securely fixing the barrier membrane prevents micromovements that can disrupt bone formation.
- Graft Stability: Ensuring that the bone graft remains in place and is adequately supported by the surrounding bone structure promotes effective integration and regeneration.
Bone Graft Materials: A Closer Look
A comprehensive understanding of the various bone graft materials used in GBR is essential for selecting the most appropriate option based on clinical needs and patient-specific factors.
Autogenous Bone Chips
Autogenous bone chips are small fragments of bone harvested from the patient’s own body, offering high osteogenic potential.
- Harvesting Sites: Commonly sourced from the mandibular ramus, iliac crest, or other accessible skeletal sites.
- Applications: Ideal for filling small to medium-sized defects and enhancing bone regeneration in conjunction with barrier membranes.
Bovine Bone Mineral
Bovine bone mineral is a widely used xenograft material known for its excellent scaffold properties.
- Processing: Treated to remove organic components, reducing the risk of immune reactions.
- Benefits: Provides a stable and biocompatible framework for new bone growth, with a slow resorption rate that supports long-term bone regeneration.
Synthetic Hydroxyapatite
Synthetic hydroxyapatite is a bioactive material engineered to mimic the mineral component of natural bone.
- Properties: Highly biocompatible, osteoconductive, and customizable in terms of porosity and structure.
- Advantages: No risk of disease transmission, customizable properties to match patient needs, and excellent integration with natural bone.
Healing of Bone Defects
The healing of bone defects through GBR involves coordinated biological processes that restore bone integrity and functionality. Understanding these healing patterns is essential for optimizing treatment protocols and ensuring successful outcomes.
Alveolar Bone Regeneration
Alveolar bone regeneration focuses on restoring the bone surrounding the teeth, crucial for supporting dental implants and maintaining oral health.
- Importance: Ensures the stability and functionality of dental implants, preventing implant failure and promoting long-term success.
- Techniques: Incorporates ridge preservation, horizontal and vertical ridge augmentation, and the use of appropriate graft materials and membranes.
Cortical Bone Healing
Cortical bone healing addresses the regeneration of the dense outer layer of bone, providing structural strength and support.
- Challenges: Cortical bone regeneration requires precise surgical techniques and the use of robust graft materials to achieve mechanical stability.
- Approaches: Utilizes non-resorbable membranes and titanium mesh to support cortical bone regeneration, ensuring effective integration and strength.
Mandibular Bone Grafts
Mandibular bone grafts focus on restoring bone in the lower jaw, essential for supporting dental implants and maintaining facial structure.
- Clinical Applications: Addressing mandibular defects caused by trauma, tooth loss, or congenital anomalies.
- Graft Materials: Often involves autogenous bone grafts or biocompatible synthetic materials to ensure effective regeneration and integration.
Predictable Bone Regeneration
Achieving predictable bone regeneration is a primary goal in GBR, ensuring consistent and reliable outcomes for patients undergoing bone augmentation procedures.
Factors Influencing Predictability
Several factors contribute to the predictability of bone regeneration, including graft material selection, membrane type, surgical technique, and patient-specific factors.
- Graft Material: Selecting the appropriate graft material based on the defect size, location, and patient health enhances predictability.
- Membrane Type: Choosing between resorbable and non-resorbable membranes based on clinical indications ensures effective bone regeneration.
- Surgical Technique: Meticulous surgical execution, including precise membrane placement and graft stabilization, promotes consistent outcomes.
Clinical Protocols
Adhering to established clinical protocols and guidelines ensures that GBR procedures are performed systematically, enhancing predictability and success rates.
- Standardized Procedures: Following standardized surgical protocols minimizes variability and promotes consistent bone regeneration.
- Continuous Monitoring: Regular follow-ups and monitoring allow for timely interventions if any issues arise, ensuring optimal outcomes.
Advanced Techniques in Bone Regeneration
Advancements in bone regeneration techniques continue to enhance the effectiveness and efficiency of GBR, expanding its applications and improving patient outcomes.
Osteopromotive Membrane Technique
The osteopromotive membrane technique involves using membranes that actively promote bone formation, enhancing the regenerative process.
- Mechanism: These membranes release growth factors and support the migration and differentiation of osteoprogenitor cells, accelerating bone regeneration.
- Benefits: Enhanced bone formation rates, improved integration with existing bone, and increased overall success rates of GBR procedures.
Porous Titanium Membranes
Porous titanium membranes offer superior mechanical stability and biocompatibility, making them ideal for complex bone defects.
- Properties: Highly durable, allowing for effective support of bone regeneration even in challenging clinical scenarios.
- Applications: Suitable for large or irregular bone defects where additional structural support is necessary to guide bone growth.
3D Scans and Customized Membranes
Incorporating 3D scanning technology and customized membranes ensures a precise fit and optimal integration with the patient’s anatomy.
- Technology: Utilizes advanced imaging techniques to create detailed models of the bone defect, enabling the design of tailored membranes and grafts.
- Advantages: Enhanced accuracy in membrane placement, improved aesthetic and functional outcomes, and reduced surgical time.
Comparative Studies and Clinical Research
Ongoing comparative studies and clinical research are vital in refining GBR techniques and materials, ensuring that best practices are based on evidence and clinical outcomes.
Comparative Histomorphometric Studies
These studies compare different graft materials and membrane types to determine their effectiveness in bone regeneration.
- Findings: Help identify the most effective combinations of materials and techniques for specific clinical scenarios, enhancing the predictability of GBR outcomes.
- Applications: Inform clinical decision-making, guiding the selection of optimal materials and methods for bone regeneration.
Multicenter Clinical Studies
Multicenter clinical studies evaluate the efficacy and safety of GBR across diverse populations and clinical settings.
- Benefits: Provide robust data on the success rates and potential complications of GBR, contributing to the development of standardized protocols.
- Outcomes: Enhance the generalizability of research findings, ensuring that GBR techniques are effective across various patient demographics and clinical conditions.
Experimental Models
Experimental models, including studies in animals and in vitro systems, explore new materials and techniques for bone regeneration.
- Purpose: Investigate the biological mechanisms of GBR and test the efficacy of innovative graft materials and membranes.
- Impact: Drive the development of next-generation GBR technologies, improving the effectiveness and safety of bone regeneration procedures.
Healing Patterns in Bone Regeneration
Understanding the healing patterns in bone regeneration provides insights into the optimal timing and techniques for GBR, ensuring effective and sustained bone growth.
Early Healing Phase
The early healing phase involves initial bone formation and the establishment of a stable environment for subsequent bone growth.
- Processes: Clot formation, recruitment of osteoprogenitor cells, and initial bone matrix deposition.
- Clinical Implications: Ensuring a stable graft environment during this phase is crucial for successful bone regeneration.
Intermediate Healing Phase
The intermediate healing phase focuses on the proliferation of bone-forming cells and the maturation of new bone tissue.
- Processes: Continued osteoblast activity, angiogenesis, and matrix mineralization.
- Clinical Implications: Supporting these processes through appropriate graft materials and membrane types enhances bone quality and integration.
Late Healing Phase
The late healing phase involves the remodeling and strengthening of newly formed bone, integrating it with the existing bone structure.
- Processes: Bone remodeling, where woven bone is replaced by mature lamellar bone, and the final integration of the graft with the host bone.
- Clinical Implications: Ensuring adequate time and support during this phase promotes the long-term stability and functionality of the regenerated bone.
Conclusion
What is Guided Bone Regeneration? It’s a transformative technique in dental and maxillofacial surgery, offering a reliable solution for bone loss and ensuring the success of dental implants and other procedures. By understanding the intricacies of GBR—from membrane types and graft materials to biological mechanisms and surgical protocols—you can make informed decisions to enhance your oral health and achieve long-term stability.
Also Read: A Review of Medical Beauty Clinics in Tainan
FAQs
Healing typically takes several months, with initial bone regeneration occurring within the first 3-6 months post-surgery. Complete integration and maturation of the new bone may take up to a year, depending on the extent of the bone defect and the materials used.
Most individuals are good candidates for GBR, especially those preparing for dental implants or experiencing bone loss due to periodontal disease. However, factors such as overall health, smoking, and existing medical conditions can affect suitability. A thorough evaluation by a dental professional is necessary to determine candidacy.
Discomfort varies among individuals, but pain is generally manageable with prescribed medications and proper post-operative care. Temporary swelling and tenderness are common, but severe pain is rare and should be promptly addressed by your healthcare provider.
GBR is often preferred for its predictability and effectiveness, especially in cases requiring significant bone regeneration. Compared to other techniques, GBR offers a controlled environment for bone growth, reducing the risk of soft tissue invasion and enhancing the stability of dental implants.